GUEST OPINION: Sharing more of Terry Almond’s story
Published 3:10 pm Wednesday, September 8, 2021
|
Getting your Trinity Audio player ready...
|
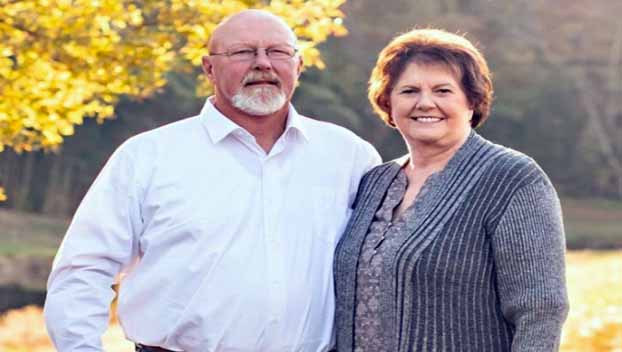
The following is by June Almond, widow of Terry Almond, the Richfield councilman who died last year after an insect sting.
Let me just say that my husband, Terry Almond, was one in a million. I always knew that, but it was confirmed to me by both a pharmaceutical company and an FDA agent this year.
Terry died on Sept. 8, 2020 from an anaphylactic reaction to an insect sting.
Only one in a million people in the U.S. die from anaphylaxis each year. Many people experience anaphylaxis, which is a sudden and life-threatening allergic reaction to something — usually food, a medication, or an insect sting. But fortunately, less than 1 percent of the anaphylactic reactions result in death. Also, the epi-pen I used failed to inject the life-saving epinephrine, and this was referenced as a one in a million unexplainable event.
I want to tell Terry’s story, hopefully to prevent anyone else from becoming this one in a million statistic. It’s a long story, but if it can help one person, it’s worth reading.
Terry was an outdoors type person — fishing, hunting, farming, whatever he could do. He had
experienced multiple insect stings over his lifetime, but he had never had a problem. About 6-8
years ago, Terry was stung by at least 20 fire ants while working on a piece of equipment at our
barn. When he started feeling strange, he got on the UTV and rode home.
When he came in the house, he was very pale, weak and sweating profusely. When I asked him what had happened, he said he got stung by fire ants. I immediately asked if he was having trouble breathing and he said he didn’t think so. The only thing I had at home was Benadryl because this was his first reaction, so I gave him some.
Since I’m a retired nurse practitioner, I was able to get my stethoscope and listen to his lungs and heart. Terry never had difficulty breathing, and he started to feel better in just a short while. His color came back, and the profuse sweating improved. But then he started complaining of chest pain. I was concerned that he might be having a heart attack from all this.
I called 911 and gave him an aspirin as they advised. When EMS arrived, they monitored him for about 30 minutes. His chest pain subsided, his vitals were stable and he felt back to normal. He didn’t want to go to the ER because he felt fine. He never received epinephrine, but I requested an epi-pen prescription from his doctor the next day.
The first epi-pen Terry received was manufactured by Mylan. It came with a trainer which has no active epinephrine so patients can practice giving themselves an injection. So, we practiced but he didn’t feel comfortable with it. Terry had a tremor of his hands, and this made handling small items difficult. If he was upset or frustrated, his shaking got worse. He remembered how weak and shaky he was with the fire ant bites, and he just didn’t believe he would have the manual dexterity to use an epi-pen.
We talked multiple times about how dangerous this could be and that he might be miles away from home when he needed the pen. I never was able to convince him, but he did agree to carry some Benadryl and take immediately if he got stung.
Since Benadryl takes about 30 minutes to work, it is not the recommended first line of treatment in anaphylaxis. Epinephrine should be given immediately. But maybe Benadryl would buy him a little time.
About 3-4 years ago, Terry was doing something in the yard, and he got stung by a wasp. He walked right in the house, again pale, weak and profusely sweating. I asked if he was having trouble breathing, and he mumbled either “I don’t know” or “I think so.”
I immediately got the epi-pen and gave him an injection. He was back to normal within about 2-3 minutes. He never experienced trouble breathing with this episode. When I first started in nursing, people were told to not administer epinephrine unless someone had problems breathing. That thinking has changed — epinephrine needs to be administered as soon as possible to save lives of those affected with serious reactions.
Around this time, there was a shortage of epi-pens and they jumped in price from about $50 to over $600. Even with great insurance, it was $300 out of pocket. One company had the monopoly, and they could charge what they wanted to. Many people couldn’t afford this lifesaving medication. Other companies started manufacturing epi auto injectors and this helped with the shortage and brought the price back down. I know there are at least five pens on the market now, and they all work differently.
Aug. 22, 2020, started out as a typical hot summer Saturday. Terry put up some outdoor security cameras that afternoon and mowed our yard and the church yard. I have a video from the newly-installed security camera of him putting up the ladder he had used at 5:48 p.m. He walked out of the building with his trademark cigar in his mouth. He didn’t seem to be in any distress or hurry, but then he got out of camera range.
At 5:55, he walked into the house, sat down in the recliner and said, “I got stung — help me open this.” He needed help opening the container that held his Benadryl. He was pale, shaky, weak with sweat pouring off his whole body. I opened the Benadryl and immediately got the epi-pen which was lying on the kitchen countertop less than six feet away. I had picked up a new prescription a couple weeks earlier.
When I took it out of the CVS bag, I noticed the pen was different and not the pen we had practiced. The instructions were on the back of the box, and it had to be removed from the carrier tube, two blue end caps removed, injected and held in place for 10 seconds in order to deliver the medication. I followed these instructions and gave the epi-pen within 30-45 seconds of him coming into the house. Epinephrine works immediately after an injection. But Terry didn’t get better, and he started having trouble breathing and turning blue. I looked at the injection site, but there was no evidence the needle had come out and injected the epinephrine. I repeated the same process again, but there was no improvement, and no evidence the needle had worked the second time. I could see the skin indention where I had put the pen against his thigh, but there was no blood visible from a puncture site.
I had another Amneal pen, but instead I got the old Mylan pen out of the cabinet and injected him with it. It functioned correctly, and I saw some blood from the puncture site, so I know the medication was injected. I was able to call 911 and get help on the way, and I began CPR. I believe all this happened in within 2-3 minutes. Three officers from the sheriff’s department arrived shortly.
They took over CPR and first responders and EMS arrived within minutes and continued with resuscitation. Terry was in cardiac arrest, and they worked so hard to get him back. He was transferred to Atrium Stanly and airlifted to CMC main.
He remained in ICU on a ventilator for about four days. Terry showed some initial improvement when the ventilator tube was removed by saying a few words and following instructions. Our family was blessed because he knew us, and he was able to tell everyone he loved us. But then he developed major complications and passed away 17 days after being stung.
Terry experienced a rapid and severe allergic reaction, and the Amneal pen didn’t function properly. I will never know if there would have been a different outcome if the pen had worked correctly the first time. I questioned myself if I should have tried another pen instead of the same one twice. I questioned myself if I could have done anything differently. I questioned myself about everything.
I started doing some research on epinephrine auto injectors when I was ready to face some of the answers to my questions.
With a simple Google search, I found multiple reports of epinephrine auto injectors not working properly. But I didn’t know that, and I don’t think others do either. Epinephrine is a lifesaving drug and should be easy for anyone to use. Children with severe allergies carry epi-pens and are taught to use them.
Between 2016-2020 both Mylan and Amneal recalled certain lots of auto injectors for problems resulting in device failure. The Pfizer and Mylan companies issued letters to healthcare providers on March 23, 2020, that devices might fail if the safety cap is removed with one hand causing some sideways force. In an emergency situation if you or someone else is collapsing from an anaphylactic reaction, it’s difficult to hold a pen at a 90-degree angle with two hands and remove the safety cap.
In June 2020, an FDA safety alert was issued for the Amneal auto injector because some lots of the device were missing a vital part which controls the medication dosage. Research your epi-pen online, otherwise you may not be aware of problems that have been reported. I did learn that Amneal recommenders if the pen doesn’t work properly the first time, try it a second time.
I reported Terry’s pen malfunction to the FDA. Anyone can make a report to the FDA if they believe there was a problem with any kind of medical device or medication, but most people don’t know that. However, in my opinion they don’t make this report user-friendly. It isn’t easy to use their online form or get someone on the phone. It took months to even get an acknowledgement that my report was received, much less investigated. I also made a report to the Amneal Pharmaceutical Company.
Both the FDA and Amneal said there had never, ever been another report regarding this epi-pen malfunctioning by not injecting the medication.
Since I am reportedly the first person ever who experienced this, and because Amneal has such a stellar record, the FDA declined to accept Terry’s pen for independent testing. I was told if there had been at least one other report of the Amneal pen malfunctioning, the FDA would have launched an investigation by an independent party. My only choice was to send the pen back to the Amneal company for testing, and I knew what their results would be. They found no deficits in the pen and found it functioned properly in their lab. The epinephrine was still in the pen and the needle worked properly for them — no shock there! The FDA told me there was no way to know why the pen didn’t work and referred to the pen malfunction as “one in a million.”
Now, I’m not claiming to be expert at giving injections, but I am certainly experienced — I’ve given thousands of injections during my years in nursing. And if this could happen to me, it could happen to anyone.
I’ve learned some things from this horrible tragedy, and if this experience could help another family from losing a loved one, it would make Terry proud. I know the pen didn’t work correctly, but there is nothing more I can do to prove that.
Terry wouldn’t have wanted me to stress out trying to fight “Big Pharma.”
If you or a loved one has ever experienced an allergic reaction that causes hives, a widespread rash, trouble breathing or shortness of breath, lip or tongue swelling, please see an allergist if at all possible. You may benefit from immunotherapy (allergy shots) that will desensitize your allergic reaction and hopefully prevent a severe anaphylactic reaction. Allergic reactions get worse with time. If your regular doctor doesn’t suggest this, ask for a referral. I should have insisted Terry go to an allergy specialist. But I didn’t, and maybe It could have saved his life.
It’s well known that allergies tend to run in families. If you have a family member or blood relative who has experienced a severe allergic reaction, please talk to your healthcare provider about a prescription for an epi-pen for yourself. Allergies can develop at any time, and anaphylaxis can get worse with each reaction. It’s better to be safe than sorry.
Always have at least two epi-pens on hand all the time. One may not work, or if there is a severe reaction, two injections may be needed. Figure out a way to keep them with you at all times.
Keep them out of the hot sun — don’t leave them in a hot car — keep them with you even if you
have to wear a fanny pack all the time. Wear a medical ID bracelet identifying your allergy. Look at your epi-pen periodically and each time you get a new prescription. It may be different from the one you are accustomed to.
For example, the Mylan pen needs to be held in place for 3 seconds, while the Amneal pen requires 10 seconds. Both these pens are activated differently. Amneal does not furnish a trainer pen, but the company will send you one if you call them or go online and make a request. Auvi-Q pens talk to the user and give voice instructions. These pen looks more like a small cell phone, and it may be easier for children to use.
Keep up with the expiration dates and replace them as needed. If you can’t afford a pen, ask the pharmacy for a discount card. All pharmaceutical companies have patient assistance programs to help uninsured patients. There are resources available for assistance, but you need to ask.
If you have ever experienced a problem with an epi-pen or any medical device, please report it
to the manufacturer and the FDA. This is how we make changes and save lives. I really have a difficult time believing this has never happened to anyone else — but I can believe it has never been reported.
Thanks to everyone who took their time to read this.